Mapping Oxygen Transmissibility for Scleral Lenses
Back in 2012 a great group of scleral lens innovators - Langis Michaud, Eef van der Worp, Daniel Brazeau, Richard Warde, and Claude J. Giasson published a groundbreaking paper describing how to estimate the oxygen transmissibility for a scleral lens.[1] One of the ideas in the paper, is that to ensure proper oxygenation of the ocular surface, it is important to consider the permeability of the lens material, as well as the thickness of the tear film. According to the Fatt formula [2], the overall Dk/t of the contact lens/tear film system can be estimated similarly to the way a conductance of two resistors in series is calculated. Basically, given that Dk of the tear film is about 80, if the lens thickness, GP material Dk, and lens vault are known, one can calculate the amount of oxygen that is transmitted to the eye surface. Acceptable Dk values that alleviate hypoxia were determined by Morgan et al. They estimate that Dk/t value of 20 Fatt units centrally, and Dk/t value of 33 Fatt units in the periphery do not cause swelling of the cornea. [3] Alternatively, Holden-Mertz place this value at 24 Fatt units for central cornea [4] and Harvitt-Bonanno recommend Dk/t of 35 Fatt units or more for the limbal area [5].
With all the complexities of a scleral lens fitting process, it may be prohibitively time consuming for the practitioner to manually calculate oxygen transmissibility during every fit. Conveniently, Michaud et al. provide several tables, which can be used as a quick reference for estimating the corneal oxygenation.
To take this concept one step further, Gaudi Software allows you to use our Patent pending technology to visualize the oxygen transmissibility map over the entire cornea. You can vary the GP material and explore how different Dk values affects the overall oxygen transmissibility. You can also test various lens designs to see, for example, if your patient will benefit from our Gaudi OxygenTM lens design. Next few figures show examples of oxygen transmissibility maps for different scleral lens designs and materials. All three figures are for the same eye. Figure 1 shows a standard lens designed with a Dk = 125 material.
Figure 2 is the same lens designed with a Dk = 200 material. Notice, that there is a great improvement in oxygen transmissibility in the limbal zone, but the change in the mid-peripheral cornea is almost negligible. This is mainly due to the irregular shape of this eye, and the fact that the Dk/t value in that region is dominated by the tear film. It is notable, that in the limbal zone, where the clearances are minimal, the increase of the Fatt value due to the use of a large Dk material is very apparent.
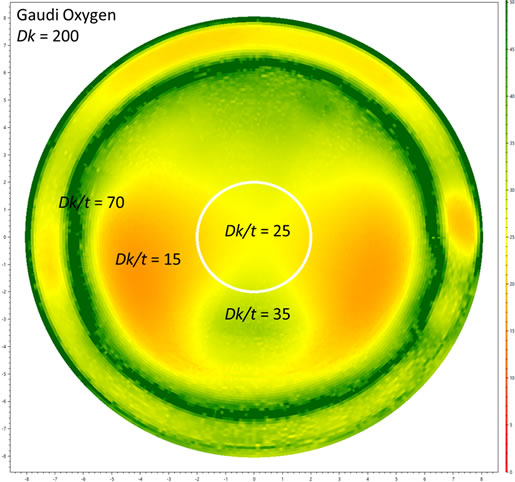
Figure 3 shows the same eye with our Gaudi OxygenTM lens with a Dk = 200 material. The design of the lens allows us to fully take advantage of the material properties and build a lens that provides a much better oxygenation of the central and mid-peripheral cornea.
References
Back in 2012 a great group of scleral lens innovators - Langis Michaud, Eef van der Worp, Daniel Brazeau, Richard Warde, and Claude J. Giasson published a groundbreaking paper describing how to estimate the oxygen transmissibility for a scleral lens.[1] One of the ideas in the paper, is that to ensure proper oxygenation of the ocular surface, it is important to consider the permeability of the lens material, as well as the thickness of the tear film. According to the Fatt formula [2], the overall Dk/t of the contact lens/tear film system can be estimated similarly to the way a conductance of two resistors in series is calculated. Basically, given that Dk of the tear film is about 80, if the lens thickness, GP material Dk, and lens vault are known, one can calculate the amount of oxygen that is transmitted to the eye surface. Acceptable Dk values that alleviate hypoxia were determined by Morgan et al. They estimate that Dk/t value of 20 Fatt units centrally, and Dk/t value of 33 Fatt units in the periphery do not cause swelling of the cornea. [3] Alternatively, Holden-Mertz place this value at 24 Fatt units for central cornea [4] and Harvitt-Bonanno recommend Dk/t of 35 Fatt units or more for the limbal area [5].
With all the complexities of a scleral lens fitting process, it may be prohibitively time consuming for the practitioner to manually calculate oxygen transmissibility during every fit. Conveniently, Michaud et al. provide several tables, which can be used as a quick reference for estimating the corneal oxygenation.
To take this concept one step further, Gaudi Software allows you to use our Patent pending technology to visualize the oxygen transmissibility map over the entire cornea. You can vary the GP material and explore how different Dk values affects the overall oxygen transmissibility. You can also test various lens designs to see, for example, if your patient will benefit from our Gaudi OxygenTM lens design. Next few figures show examples of oxygen transmissibility maps for different scleral lens designs and materials. All three figures are for the same eye. Figure 1 shows a standard lens designed with a Dk = 125 material.
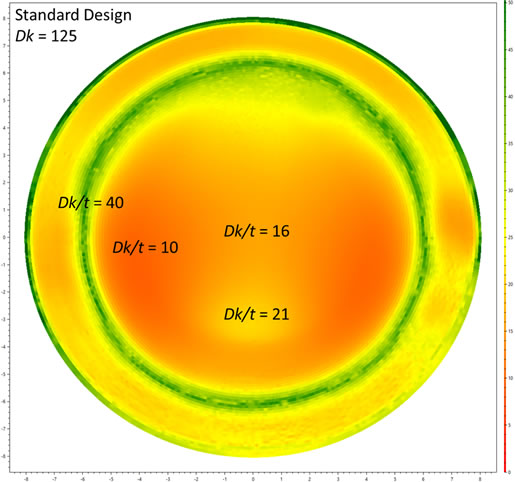
Figure 2 is the same lens designed with a Dk = 200 material. Notice, that there is a great improvement in oxygen transmissibility in the limbal zone, but the change in the mid-peripheral cornea is almost negligible. This is mainly due to the irregular shape of this eye, and the fact that the Dk/t value in that region is dominated by the tear film. It is notable, that in the limbal zone, where the clearances are minimal, the increase of the Fatt value due to the use of a large Dk material is very apparent.
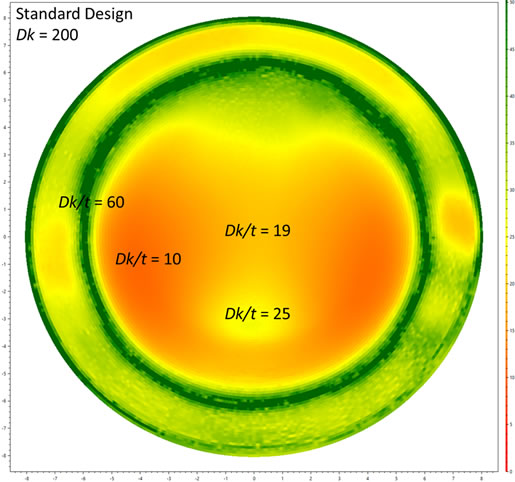
Figure 3 shows the same eye with our Gaudi OxygenTM lens with a Dk = 200 material. The design of the lens allows us to fully take advantage of the material properties and build a lens that provides a much better oxygenation of the central and mid-peripheral cornea.
References
- Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012 Dec;35(6):266-71.
- Fatt I. Oxygen transmissibility considerations for a hard-soft contact lens combination. American Journal of Optometry and Physiological Optics 1977; 54: 666–72.
- Morgan PB, Brennan NA, Maldonado-Cordina C, Quhill W, Rashid K, Efron N. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye soft contact lens wear. Journal of Biomedical Materials, Research Part B: Applied Biomaterials 2010;92(February (2)):361–5.
- Holden BA, Mertz GW, McNally JJ. Corneal swelling response to contact lenses worn under extended wear conditions. Investigative Ophthalmology and Visual Science 1983; 24: 218–26.
- Harvitt DM, Bonanno JA. Re-evaluation of the oxygen diffusion model for predicting minimum contact lens Dk/t values needed to avoid corneal anoxia. Optometry and Vision Science 1999; 76(10): 712–9.